10.1 PreLab Reading – Urinalysis
Overview
The kidneys play a crucial role in maintaining the body’s water and salt balance, removing metabolic waste, regulating blood pressure, and stimulating red blood cell production. The urinary system has six primary functions:
- Regulation of ion concentrations in blood plasma
- Regulation of plasma volume and blood pressure
- Regulation of plasma osmolarity
- Regulation of acid-base balance
- Regulation of metabolic waste products and substances such as drug metabolites
- Secretion of erythropoietin and renin, and activation of Vitamin D3 to calcitriol
Urine Formation
Urine formation involves three main steps:
- Filtration: Blood plasma is filtered to form filtrate.
- Reabsorption: Water, ions, and reusable molecules (e.g., glucose) are reabsorbed back into the blood.
- Secretion: Chemicals, including waste products and hydrogen ions (H+), not removed during initial filtration are secreted into the filtrate.
Once these steps are completed, urine is excreted from the body through micturition (urination). The kidneys process around 180 liters (about 50 gallons) of filtrate daily, filtering the total plasma volume approximately 60 times per day. Most of the filtrate (99%) is reabsorbed, resulting in the production of only 1-2 liters of urine per day. These processes enable the kidneys to effectively filter and maintain the body’s internal environment.
The functional unit of the kidney is the nephron, which produces urine through filtration, reabsorption, and secretion. The nephron consists of:
- Renal corpuscle: includes the glomerulus (full of capillaries) and Bowman’s capsule
- Proximal convoluted tubule
- Loop of Henle
- Distal Convoluted tubule
The first step is urine formation is filtration, where blood plasma is filtered in the glomerulus. Water and small substances move from the glomerulus into Bowman’s capsule to form filtrate, while red blood cells, white blood cells, platelets, and plasma proteins remain in the blood.

Urine Color. Figure by https://pressbooks.ccconline.org/bio106/chapter/muscular-levels-of-organization/
Many plasma components that enter the filtrate are useful for body functions and are reabsorbed back into the blood. Reabsorbed components include water, ions (Na+, K+, Cl-, Ca2+, HCO3), glucose, amino acids, and water-soluble vitamins. Reabsorption occurs mainly in the proximal convoluted tubule but also in the loop of Henle, distal convoluted tubule, and collecting duct (which is technically not part of the nephron).
Since only about 20% of the blood plasma is filtered during a single passage through the kidneys, not all waste products are initially removed. Waste products such as creatinine, urea, drugs, and excess ions like K+, and H+ (important in regulating acid-based balance) are secreted from the peritubular capillaries into the renal tubules. Secretion occurs in the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct. After urine is formed through these processes, it is excreted from the body by micturition (urination).
Here are some tests used to assess kidney function and diagnose urinary system or other diseases:
- Blood Tests
- Serum Creatinine: Measures creatinine, a waste product from muscle breakdown. Elevated levels indicate impaired kidney function and can help estimate the glomerular filtration rate (GFR).
- Blood Urea Nitrogen (BUN): Assesses the concentration of urea, a waste product from protein metabolism. Increased BUN levels suggest kidney dysfunction.
- Hematocrit: Evaluates red blood cell levels. Low hematocrit can indicate anemia, which is chronic renal failure to reduce erythropoietin production by the kidneys.
- Urine Tests
- Urine Culture: Identifies bacterial species in the urine and determines the effectiveness of antibiotics for treating infections.
- Urinalysis: Involves a dipstick test and microscopic examination. It can detect kidney failure, urinary tract infections, kidney stones, diabetes, and liver disease.
The dipstick contains chemicals that react with substances in the urine, changing color to indicate the presence of blood, protein, leukocytes, nitrites, glucose, ketones, bilirubin, and urobilinogen. It also measures pH and specific gravity.
Here’s is a more concise and refined explanation of some key aspects evaluated in a urinalysis:
Color: The yellow color of urine is due to urobilinogen, a breakdown product of heme from red blood cells. Bilirubin is first excreted into the intestine and then converted to urobilinogen, which is reabsorbed into the blood and excreted in urine. Urine color can vary based on hydration, diet, and certain medical conditions.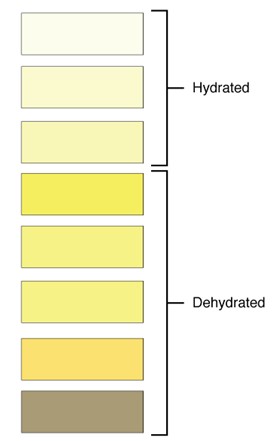
Urine Color. Figure by https://pressbooks.ccconline.org/bio106/chapter/muscular-levels-of-organization/
Clarity: Urine is normally clear. It may become cloudy if allowed to stand or if it is contaminated by bacteria, which may indicate a urinary tract infection (UTI).
Odor: Fresh urine typically has a mild odor. When urine stands, it can develop a more “ammonia-like” smell. Diet (e.g., asparagus) and certain medical conditions, such as UTI, can also affect urine odor.
pH: Normal urine pH ranges from 4.5 to 8, with an average around 6. pH can be influenced by diet and health conditions. For instance, a low pH may indicate compensation for respiratory acidosis, while a high pH might reflect compensation for respiratory alkalosis. Excess vitamin C intake can also lower urine pH.
Specific Gravity: This measures the density of urine compared to water (specific gravity of 1.000). Normal ranges are from 1.003 to 1.032. Specific gravity can be affected by fluid intake, diet, and health conditions. For example, in chronic renal failure, the specific gravity may be low due to decreased water reabsorption by the kidneys.
Urobilinogen and Bilirubin: These tests help determine the presence of liver disease or hemolysis. Elevated urobilinogen levels may suggest liver issues, while bilirubin in urine could indicate liver dysfunction.
Leukocytes: Increased leukocytes suggest a UTI. Pyuria, or an elevated number of white blood cells in the urine often indicates infection.
Nitrites: Elevated nitrite levels can signal a UTI, as certain bacteria produce nitrites.
Blood: Normally, urine should not contain red blood cells (RBCs). Hematuria, or blood in the urine, can be caused by UTIs, kidney or bladder stones, prostate issues, bladder cancer, trauma, strenuous exercise, or glomerulonephritis.
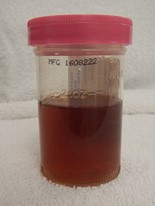
Hematuria: Blood in urine. Figure by https://pressbooks.ccconline.org/bio106/chapter/muscular-levels-of-organization/
Protein: Normally, urine contains minimal protein. Proteinuria, or excess protein in urine, can result from fever, illness, exercise, dehydration, or stress. It may also indicate more serious conditions like glomerulonephritis.
Glucose: Urine should not contain glucose, as it is typically reabsorbed in the proximal convoluted tubules. Glucosuria, or glucose in the urine, is often associated with diabetes mellitus or certain kidney diseases.
Ketones: Normally absent from urine, ketones can appear in conditions such as poorly controlled type 1 diabetes mellitus, starvation, or when following a ketogenic diet.
Questions
-
- What substances do the lungs receive from the circulatory system, and what do they supply to it?
- How are water, ions, and reusable molecules (e.g., glucose) returned to the blood during kidney function?
- What is the first step of urine formation called, and what happens during this process?
- What are the normal characteristics of urine?
- What is the term used to describe the presence of blood in urine, and what might cause it?
Adapted from Human Physiology Lab Manual by Jim Blevins, Melaney Farr, and Arleen Sawitzke, Salt Lake Community College.

