9.1 PreLab Reading – Spirometry
Overview
The respiratory system facilitates the exchange of O2 and CO2 between the atmosphere, the body, and its cells, enabling the intake of O2 for aerobic respiration and the release of CO2 for regulating body fluid pH. In this lab, we will examine lung ventilation to understand how air is exchanged between the alveoli and the atmosphere. The amount of air in the lungs during ventilation varies significantly depending on which muscles are driving airflow and the force of their contractions. The different volumes of air moved in and out of the lungs by contracting different muscle groups are known as primary lung volumes. Combinations of these lung volumes give us lung capacities, which indicate how much air is present in the lungs or can be moved by the lungs under specific conditions.
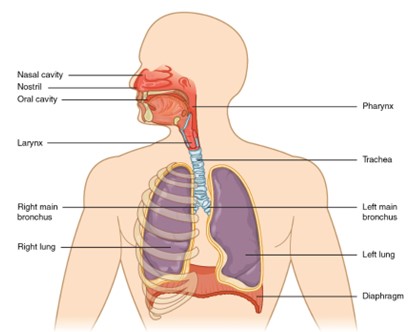
Structures of the Respiratory System: Nasal cavity, oral cavity, pharynx, larynx, trachea, bronchus, lungs, and diaphragm. (Figure by OpenStax is used under a Creative Commons Attribution license.)
Respiration is the process by which the body obtains and utilizes oxygen and produces and eliminates carbon dioxide. It can be divided into five stages:
- Pulmonary Ventilation: The movement of gases between the lungs and the environment. This will be studied in this lab.
- Pulmonary Gas Exchange: The movement of gases within the bloodstream.
- Gas Transport: The movement of gases within the bloodstream.
- Tissue Gas Exchange: The movement of gases between the bloodstream and the tissues.
- Cellular Respiration: The consumption of oxygen and the production of carbon dioxide by the mitochondria inside body cells.
The human respiratory system consists of a series of tubes that branch out and end in clusters of small membranous air sacs called alveoli. During pulmonary gas exchange, oxygen and carbon dioxide diffuse between the alveoli and the capillaries through the respiratory membrane, which is two cell layers thick – the epithelial cells of the alveoli and the epithelial cells of the capillary. Factors influencing gas diffusion include surface area, diffusion distance, and concentration gradient. The total area of the alveoli is approximately the size of a tennis court, and their think walls provide a short diffusion distance. A high concentration gradient is maintained by 1) the movement of blood with low oxygen and high carbon dioxide levels to the lungs, and 2) pulmonary ventilation (breathing), which ensures, high oxygen levels and low carbon dioxide levels in the alveolar air. Therefore, the alveoli and associated blood supply are well-suited for the diffusion of oxygen into the blood and carbon dioxide from the blood into the alveoli.
Lung ventilation is produced by muscular contractions. The resulting change in thoracic volume is transmitted to the elastic lungs via the fluid-filled pleural cavity. Inspiration (inhalation) is achieved by the contraction of the diaphragm and the external intercostal muscles, both of which increase the volume of the thoracic cavity. In a resting individual, expiration (exhalation) is typically passive as muscle relaxation and lung elasticity allow a decrease in thoracic volume. During exercise or other strenuous activities, forced expiration is produced by the contraction of the internal intercostal and abdominal muscles.
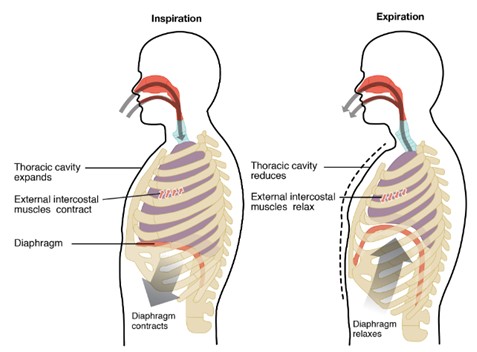
Inspiration and Expiration: muscles involved during inspiration and expiration. (Figure by OpenStax is used under a Creative Commons Attribution license.)
The change in lung volume during inspiration and expiration causes a change in intra-alveolar pressure (Palv), which is the pressure of the air inside the alveoli. During inspiration, lung volume expands, causing Palv to decrease to -1 mmHg (as gas molecules spread out in a larger volume, pressure decreases). Conversely, during expiration, lung volume decreases, causing Palv to increase to +1 mm Hg (as gas molecules crowd together in a smaller volume, pressure increases). This inverse relationship between pressure and volume is described by Boyle’s Law, written as P = 1/V.

Boyle’s Law: Pressure and volume inversely proportional. (Figure by OpenStax is used under a Creative Commons Attribution license.)
Air flows into and out of the lungs along its pressure gradient from high pressure to low pressure. During inspiration, atmospheric pressure (Patm) outside the body is at 0 mm Hg (standardized for ease of calculations, though it is actually 760 mm Hg at sea level), while Palv is -1 mm Hg, so air moves into the lungs down the pressure gradient from 0 to -1 mm Hg. During expiration, as lung volume decreases, Palv increases to +1 mm Hg, which is higher than Patm, causing air to move out of the lungs.
Two other important lung pressures are intrapleural pressure, the pressure within the pleural space, and the transpulmonary pressure, the pressure across the lung wall and the force for lung expansion. The transpulmonary pressure is calculated as alveolar pressure minus the intrapleural pressure. The higher the transpulmonary pressure, the more expanded the lungs are. If this pressure were 0, lung volume would collapse.
Ventilation volume and rate are controlled by the respiratory control centers in the medulla oblongata and pons of the brainstem. These centers ensure that the exchange of oxygen and carbon dioxide at the lungs matches the body’s requirements. For example, carbon dioxide release during expiration is closely linked to the role of the respiratory system in pH homeostasis. Respiratory control is dynamic, adjusting to the body’s changing needs over time. The respiratory control centers match the oxygen used and carbon dioxide produced by tissues with the oxygen uptake and carbon dioxide discharge at the lungs. Lung ventilation is influenced by various factors, including emotions, speech, disease, and body position relative to gravity.
Spirometry, Lung Volumes, and Lung Capacities
A spirometer is a device used to measure lung volumes, calculate lung capacities, and measure airflow rates, which are essential for diagnosing lung diseases. Several types of spirometers can be used:
- Wet Spirometer: Utilizes water to form a low-friction seal between a bell float chamber and the environmental air. As the patient breathes in and out, the rise and fall of the bell are recorded.
- Dry Spirometer: Often used in clinics or hospitals to assess a patient’s respiratory function.
- Sanborn Respirometer: Measures lung volumes and oxygen consumption.
- Computerized Spirometer: Most modern spirometers are computerized for enhanced accuracy and data analysis.
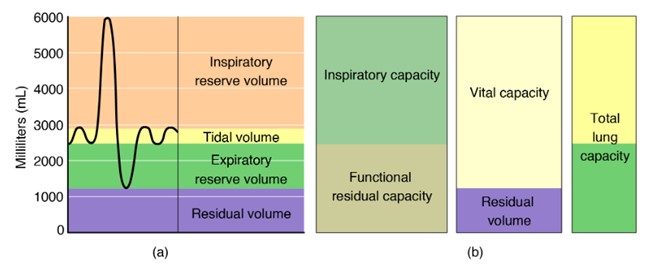
Spirometry: Lung volumes. (Figure by OpenStax is used under a Creative Commons Attribution license.)
The graph generated by a spirometer is called a spirogram, which is used to determine lung volumes and capacities.
Lung Volumes
- Tidal Volume (TV or VT): The amount of air that moves in or out of the lungs during a single breath at rest.
- Inspiratory Reserve Volume (IRV): The volume of air that can be forcibly inhaled above the normal tidal volume.
- Expiratory Reserve Volume (ERV): The volume of air that can be forcibly exhaled following a normal tidal expiration.
- Residual Volume (RV): The volume of air remaining in the lungs after maximal forceful expiration (this cannot be measured by a spirometer).
Lung Capacities
Lung capacities are calculated by combining different lung volumes:
- Inspiratory Capacity (IC): The maximum of air that can be inhaled after a normal tidal expiration.
- Vital Capacity (VC): The amount of air that can be inhaled and then exhaled with maximum effort.
- Functional Residual Capacity (FRC): The amount of air left in the lungs after a normal tidal expiration.
- Total Lung Capacity (TLC): The maximum amount of air the lungs can contain (average = 6,000 ml).
These are values based on a healthy 70 kg adult male. Lung volumes vary by age, gender, height, and ethnicity. Generally, women have smaller lung volumes than men, and lung volumes decrease with age due to decreased lung elasticity. Tidal volume also increases during exercise to meet the higher oxygen demand of the muscles.
Diagnosing Lung Disorders
Spirometry can detect abnormalities in lung volumes and capacities, indicating lung diseases, which can be obstructive or restrictive.
- Obstructive Lung Disease: Airways are inflamed, narrowed, and can collapse, obstructing airflow during exhalation. This increases residual volume (RV) and causes overinflation, raising functional residual capacity (FRC) and total lung capacity (TLC).
- Restrictive Lung Disease: Lungs do not expand properly, decreasing vital capacity (VC) and total lung capacity (TLC). This can be due to decreased lung compliance, a deformed chest cavity, or weak breathing muscles caused by neuromuscular disorders.
The Forced Expiratory Volume in 1 second (FEV1) measures the percentage of the Forced Vital Capacity (FVC) exhaled in one second, indicating whether the airways are obstructed. To distinguish between asthma and COPD, a bronchodilator is administered; an increased in FEV1 by 12% or more indicates asthma. The FEV1/FVC ratio helps differentiate between obstructive and restrictive lung diseases when FEV1 is decreased.
Questions
-
- What substances do the lungs receive from the circulatory system, and what do they supply to it?
- How do the lungs interact with the atmosphere during breathing in terms of the substances they receive and exhale?
- What happens to the volume and pressure in lungs during inhalation?
- What changes occur in the volume and pressure of the lungs during exhalation?
- How would you define the following respiratory terms:
- Tidal Volume
- Total Lung Capacity
- Inspiratory Reserve Volume
- Expiratory Reserve Volume
- Residual Volume
- Functional Residual Capacity
- Forced Vital Capacity
- FEV1
Adapted from Human Physiology Lab Manual by Jim Blevins, Melaney Farr, and Arleen Sawitzke, Salt Lake Community College.

